The Improvement Dilemma
Being highly time critical and expensive, Clinical Development has been and still is a target of constant improvement. Every mature pharmaceutical and maturing biotech company with established or evolving clinical organization builds-up one or more process-, operational excellence- or continuous improvement-groups to tackle their persistently unfulfilled vision of efficiency in this area.
Despite enormous efforts, we are faced daily with the perception of business leaders, that clinical development operations systematically are inefficient, labor-intensive, too expensive and do not cope with the needed innovations and speed in pharmaceutical development.

Despite all efforts, things got worse
Contradicting all past streamlining exercises and efforts to automate, things only got worse.
Few but striking examples are:
- Clinical Trial Management Systems (CTMS) are outdated systems, that track trial activities with significant delay between data collection and entry of the data in the CTMS. Visit reports are recorded in documents without interface to dependent systems. Improvement efforts in the CTMS space led in contrast to intention to increased complexity and lower user compliance. In the end, the data quality problems remain.
- The introduction of eCRF (EDC) promised us the end of data clarifications, we have more queries in data cleaning than ever before.
- Clinical Supplies remains as a basic & enabling process and despite large investments in inter-operability, an un-integrated, firefighting and individual dependent activity.
- Contrasting to the forceful introduction of eTMFs, we have not been able to reduce the time spent on misplaced documents, nor establishing homogeneity among all investigator files. Audit readiness remains the unachieved goal.
- Notwithstanding huge investments in analytics concepts, platforms and tools, we still struggle with data sets at the end of a study, often requiring multiple rounds of rework. Still today, valuable data points need to be dropped due to missing timestamps, in turn impacting the quality and validity of the filing This all despite data lakes, data cubes and what not more.
Obviously, there are serious improvement inabilities with regards to the highly inefficient clinical development.
Many blame the lavish earnings or the dominance of medical scientists for the lack of progress. This however doesn’t hold up, as some companies with no earnings or with an ailing pipeline also have the same problem. Moreover, the aforementioned improvement departments are filled with non-medical experts.

The “Improvement Dilemma”
We believe there is an Improvement Dilemma in play. The dilemma in improvement strategy consists of the dogma that incremental improvements would solve the underlying problem better than disruptive end-2-end focused changes. With this philosophical, unempirical and misleading paradigm, which is and always have been driven by mind-making, influential groups detached from real business operations and detached from actual considerations of implementation efficiency, we lost the ability to lift our view and fundamentally question the root cause of the issue and consequentlyidentify the major opportunity to improve. The take away is, that by improving incrementally, you do not advance fundamentally, because you stick to the underlying base of the weakness and the existing way of doing, which apparently failed.
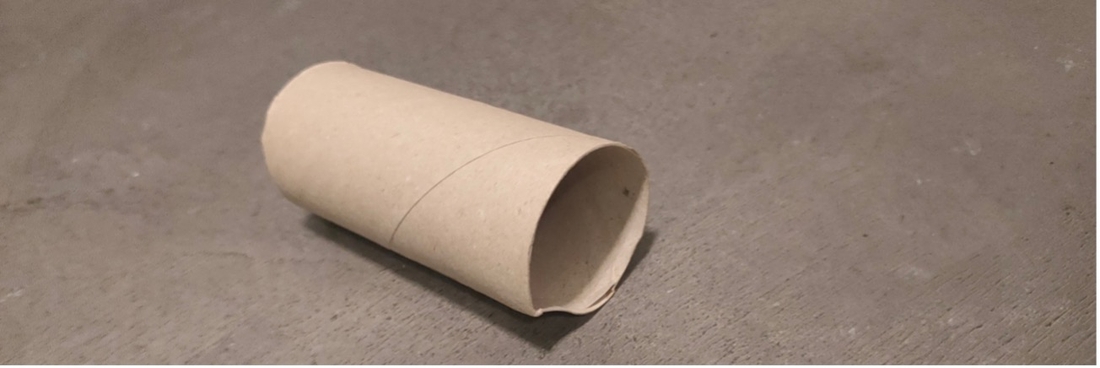
Illustrative for an Improvement Dilemma is the well-known toilet roll. The inner core of toilet rolls is a tube simply made of carton, useless for the customer, inside the roll of paper. The roll of paper ultimately is the only part of added value for the customer. The tube requires a separate and distinct manufacturing process with its own materials. When the paper is used, the carton roll needs to be disposed, often an activity full of conflict in homes with teenagers by the way.
Through the years we saw the tubes getting thinner, less bleached but not fundamentally changing. It was incremental improvements not solving the problem for the customer but called-out as improvement. Until recently, when we bought new toilet paper and were astonished to see a real improvement: no tube inside the roll anymore.
Someone had taken a step back and questioned the fundamental: do we -still- need a tube, does the customer -still- need a tube? And indeed, we can do without. The tube does not add any value, it is a relic from the past. That is a change, which positively disrupts the customer experience of something common such as toilet paper. The industry needed decades for such an obvious “disruptive” improvement of customer experience and efficiency.
The Toilet Roll Tube of Clinical Development
Let us apply this to the tube of clinical research: the Clinical Trial Management System or short CTMS. Every company has one. And every company struggles with CTMS data timeliness, completeness, quality and accuracy.
Multi-millions have been spent on finding solutions. None of projects truly resolved the fundamental issues. CTMS is still a redundant system, where we reproduce data from other systems or documents such as the protocol, and so on. The CRA’s still fill in the data, often in the hotel and in the evening after a full day of monitoring. If they fill it in at all or in sufficient completeness.
We are busy to continuously improve an outdated, pre-internet system. We thereby forget to step back and look for the real innovation. Just like with the toilet roll tube, we should escape the Improvement Dilemma. Taking a step back, not jumping to improve each and every flaw, without asking the only senseful question with a real impact: do we still need a CTMS?
Taking the Tube out of Clinical Development
The disruptive and real innovation is to change to a comprehensive end-2-end interoperability. Can we take out the “tube CTMS”? The post-fact tracking systems has no real value. Let’s leverage the tools already in place, which actively direct and control the study: IRT, intelligent clinical supply management, and advanced Data Collection Tools. Adding – low-code – smart workflows can improve the whole monitoring experience, timeliness and quality.
How we imagine this innovation? Follow our articles in Clinical Trials Arena to find out.
The Improvement Dilemma: by improving incrementally you don’t fundamentally advance because you stick to the underlying flaws of the as-is system and the existing way of doing.
Stay up to date with the latest #Lifeattenthpin #LifeSciences #Pharma #MedDevices #Biotech #Digitalforlife #Thoughtleadership #Medical Technology #AnimalHealth news by following us on Instagram #LifeAtTenthpin Facebook Tenthpin and our Tenthpin LinkedIn corporate page.


