Pursuing Excellence in Clinical Supply Management – Topic 2: End to End Visibility
Tenthpin has launched a short series of articles covering aspects of differentiation and excellence for clinical supplies management. These articles are collections of experiences and insights which have come from working with the industry on various initiatives over many years. At Tenthpin, we have enormous respect and often awe at the achievements and impact of clinical supply chain professionals across the globe, and we offer this content as a way of illuminating and perhaps enhancing their performance. What follows is Article 2: End to End Visibility. Upcoming articles in this series will examine planning excellence, and business intelligence.

Introduction
Clinical Supplies remains, despite large investments in inter-operability, as a basic and enabling process, an un-integrated, firefighting and individual dependent activity.
The operational conduct of clinical supplies is a multi-dimensional activity. Its success deeply relies on an organized information flow and time-sensitive activities of several functions usually located in the clinical operations, the technical research & development, regulatory organizations and the clinical supply operations.
The foundational information flow however appears to be often interrupted due to silo-ed functions and not coordinated activities and communication.
As a result, the clinical supply operations appear as highly inefficient with a lot of noise, escalations and organizational hick-ups. Moreover, resources are wasted on automatable tasks, on redundant tasks, on re-work, on operational frictions, and on overhead.
Finally, the output is suboptimal and results in long planning cycles, too high security buffers, delays and worst of all: patients without drug.
Attempts to improve the highly complicated and inter-dependent process often focuses on optimization of parts instead of optimizing end-to-end visibility, network interdependencies and the crucial but limited number of steps of real impact to entire supply chain performance. Focusing on partial improvements and steering of only portions of the entire business and operational process-network leads to problems on the end-to-end level (see article The Improvement Dilemma).
The goal to achieve end-to-end visibility therefore is a comprehensive, multi-dimensional effort solved by coordinated actions on system integration, workflow optimization and optimized communication organization.
Interdependencies in the Process
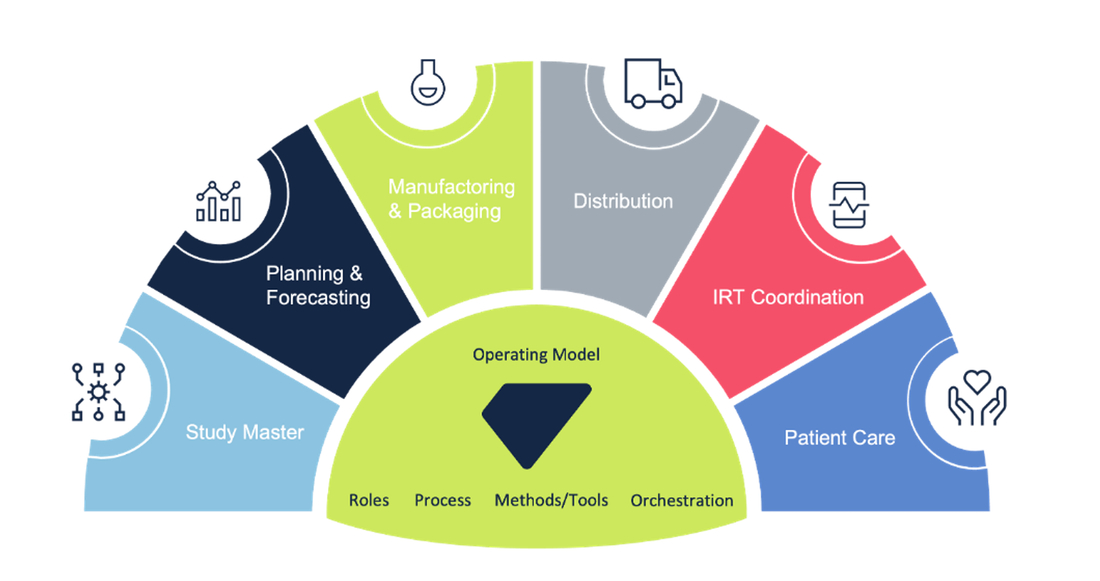
A clinical supply chain consists of many specialized activities, each of which is dependent on the other in terms of time and success. In the process, many physical items, as well as information, need to come together at the right time from many sources, often from organizationally separated business departments.
During the set-up phase of the clinical supply chain, many of these items, starting with the drug substance (DS) through the formulated drug product (DP) and the dosage form, as well as the packaging design on a primary and secondary level, are still in technical development and the regulatory approval process. The same goes for much of the details related to the compound directly or indirectly like export documentation and labelling.
The activities are performed by many functions within and outside of the sponsor. Within the sponsor’s organization itself, the number of specialized departments span from research and development, clinical operations, technical development, finance, legal, and on to logistics.
We often find that the clinical operations function has limited awareness of the importance of the timely available information or timely fulfilment of prerequisites needed to support the preparatory activities to build a successful clinical supply chain. The same goes the other way around; for instance, for the clinical trial application (CTA), the specialized regulatory CTA department needs data about the drug which many in clinical supplies are not aware.
In the highly complex process, these interdependencies are very time-critical and often loosely coupled and managed. Changes in one often have an impact on other functions. Accordingly, a lot of effort is spent to collect the missing pieces, perform the required re-entry of data, and re-work and adapt settings for the supply chain.
The more the process proceeds towards the actual delivery to sites and being ready for dispensing to patients, the more time-critical the activities become. Only if all is complete, in the right quality and with comprehensive documentation, can the drug finally be dispensed to the patient. In assuring this, the checkpoints become more elaborate and frequent the closer the flow of goods proceeds towards patient dispensation.
The importance of lead times
The successful delivery of the clinical finished good (CFG – the specifically labelled medication pack being dispensed to a patient) in the right quantity, at the right time, at the right location and in the right quality depends on closely linked and interdependent steps. This process needs a guiding principle to steer it.
A guiding principle is even more crucial as the entire development portfolio results in integrated capacity requirements at the different steps of the clinical supply chain. As such, the requirements integrate on an entire portfolio level, eg. within the production scheduling and execution planning of the DS, DP and packaging production facilities.
Such a guiding principle can be generated by dividing the supply chain into certain distinct sub-process elements: for example, DS manufacturing up to the release and goods receipt at the DP production facility, DP manufacturing up to the release and goods receipt at the packaging facility, and more downstream in the process, the delivery from the regional depot to the investigator site. Each of the sub-process elements has a lead-time of fulfilment and characteristics (parameters) of successful performance. Thereby, the lead times for many sub-process elements are compound-specific, for other sub-process elements, standard lead times true for every supply chain within a particular setup are valid.
Arranging the lead times for every sub-process element in the entire supply chain has two advantages: it allows control of the interdependencies in the process and denotes the impact of delays in either deliverable by aforementioned players or proceeding step on the entire performance of the supply chain.
It is only with a comprehensive end-to-end understanding and visibility of sub-process elements and their lead times involved that these controls are truly meaningful and foster an optimization of the delivery from DS all the way to patient dispensing.
The overarching context allows an orchestration from high-level planning to actual execution and assembly.
Risk buffers – a reaction to missing end-to-end visibility
Risk buffers (often called ‘overage’) are common to every clinical supply chain, if not to every demand-driven supply chain. Often misunderstood and even criticized as ‘waste’, risk buffers are a hallmark and inevitable reaction towards the inherent dynamics of clinical development, long lead times and imperfect end-to-end visibility.
Risk buffers, in a very simplified approach, are the differences between the final consumption of a material calculated by the need of the customer and the amount of material produced along the supply chain to cope with supply chain inefficiencies. In a clinical supply chain, risk buffers are applied at every material level (DS, DP, primary and secondary packed material, CFG inventories at the depots and at investigator sites). The customer need for all this is the dispensing of CFG at the investigator site to patients enrolled in the clinical trial.
The size of the risk buffers can differ substantially from one drug under investigation to another, from one study protocol to another, and from regional allocation of one clinical trial to another – all leading to the possibility of several multiples to the actual need of the enrolled patients.
Risk buffers can be expensive and their cost increases with the increasing cost of investigational drugs. Some drivers of the size of risk buffers can be influenced, some others not – at least not without jeopardizing the scientific value of a clinical trial.
The health of a clinical supply chain increases by reducing the lead time of the availability of the materials, reducing the lead time in the distribution chain until the investigator site, and increasing the flexibility in the use of particular materials in the supply chain across different study protocols and/or across different countries and regions per the study.
Moreover, key enablers for increasing the health of a clinical supply chain are enhanced end-to-end visibility, which is then often coupled with an increasing speed in re-planning and re-arranging the supply chain due to changes to the original assumptions or updated actual patient-based results of the trial.
Risk buffers, for instance, often need to be increased in case the inventories at depots and investigator sites need to cover longer periods of patient enrollment. Such periods can be reduced only by more accurate and timely visibility into the actual enrollment at the investigator site.
The longer the lead times to re-produce materials or transport the materials along the entire supply chain, the slower one can react to changes in the assumptions, the slower one can react to what really happens at the investigator site, and again the slower one can react to incidents in the supply chain. Consequently, the risk buffers need to be even higher – at worst, as high as to cover a full lead-time from DS production until the delivery of the CFG at the investigator site.
Noteworthy, risk buffers can be decreased with increased flexibility in re-planning. Timelines of several weeks or even months to finalize re-planning, and thus react to new assumptions or incidents in the supply chain, are indicators of a substantially decreased health of a supply chain. The same is true if the frequency of the re-planning is too low (weekly or even monthly cycles).
In summary, the higher the end-to-end visibility, the more actual the end-to-end information, the shorter the lead times and finally the higher the flexibility in re-planning, the lower the risk buffers in the supply chain and, consequently, the lower the costs of the entire supply chain portfolio.
The importance of inter-operable E2E systems
In creating any sort of end-to-end planning and insights, system interoperability is fundamental. In clinical development in general, this has traditionally been an area of challenge with the many highly-specialized applications that have been developed for and with specialized users. These systems are geared towards the specific function and are rarely designed to interact with other specialized systems.
Lack of forethought leads to inconsistencies in data, a lot of redundant data, and a huge reconciliation effort when we need to ensure that the data is consistent and complete. For example, the consolidation of adverse events between the data in the EDC and the safety system is a huge effort. The same goes for the integration of laboratory metadata in analytical files.
However, having complete shared data is essential when creating an end-to-end overview and coordinating activities across a highly complex process. As we mentioned before, this shared data structure is hampered by the fact that the separate activities and systems are set up without that overarching understanding and alignment we talked about.
In order to enable a coherent view of the process and, even more importantly, be able to plan and control it, we need to establish a continuous data flow.
Establishing data and system interoperability is crucial. Next to providing the fundament for visibility and planning, it also provides users with the possibility to have (near to) real time insights and adaptation from one change to another. When we shift, for instance, the patient goal for one country to another, with an integrated system, this can immediately trigger a recalculation on the supply planning,
We can approach data interoperability in a number of ways, ranging from APIs on a filed level, to RPAs transferring data, to creating truly integrated platforms where data generation is truly aligned, streamlined and full in sync.
The more we can create a seamless data flow, the better our real-time visibility, the more up to date our planning with easiness to do replanning without the normal long rescheduling lead time upon changes within clinical operations.
Taking the interoperability a step further, we can create the next level of visibility and coordination with automation and workflow management. We then truly start to eliminate repetitive activities, reduce mistakes and have early escalation in place to pro-actively avoid delays and stockouts and, most importantly, non-treatment of patients.
Conclusion
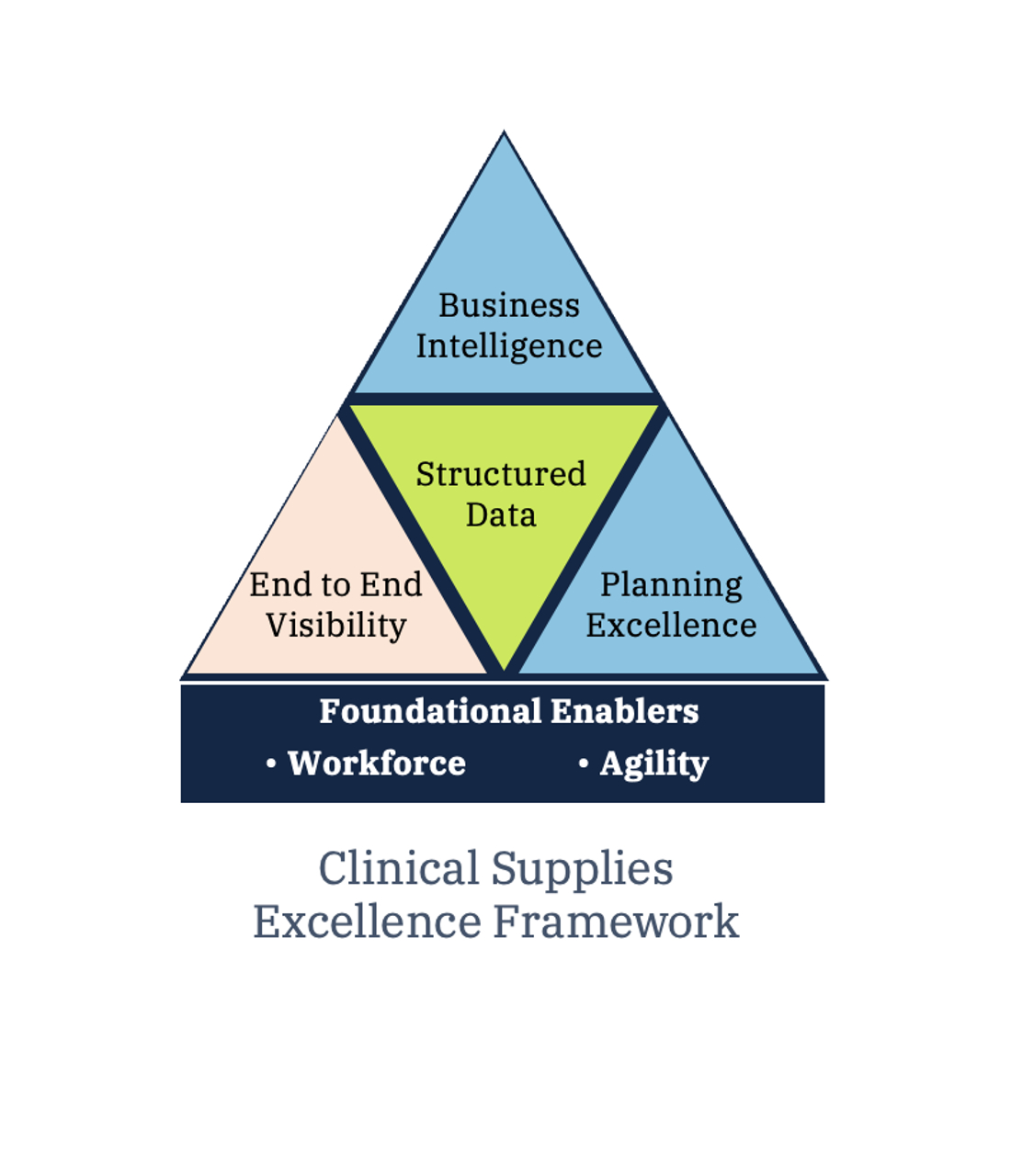
Your clinical supply workforce and their capacity to be both responsive and agile are the foundation for positive and enduring improvements in clinical supply performance. These two factors span your operational strategy and your capacity to execute it and are thus essential to the operational excellence capabilities of end-to-end supply visibility, planning excellence, and business intelligence which we will explore in successive articles. Your clinical supply workforce and their capacity to be both responsive and agile are the foundation for positive and enduring improvements in clinical supply performance. These two factors span your operational strategy and your capacity to execute it and are thus essential to the operational excellence capabilities of end-to-end supply visibility, planning excellence, and business intelligence which we will explore in successive articles.
Article has been published in Clinical Trials Arena “By Bart Reijs, Advisor at Tenthpin, and Frank Altznauer, Chief Industry Advisor at Tenthpin”
Stay up to date with the latest #Lifeattenthpin #LifeSciences #Pharma #MedDevices #Biotech #Digitalforlife #Thoughtleadership #Medical Technology #AnimalHealth news by following us on Instagram #LifeAtTenthpin Facebook Tenthpin and our Tenthpin LinkedIn corporate page.


